Advance care planning (ACP) supports patients and families in discussing and documenting care preferences, with the goal of ensuring that the care patients receive is aligned with their goals, values and priorities.
In many instances, when asked about their preferences, patients and families will prioritize remaining in the home vs. going to the hospital, and favor comfort and quality of life over invasive care that may carry limited benefits. In such situations, when patient preferences are honored, the resulting changes in the way patients engage with the health care system result in lower overall health care costs. These effects have been demonstrated in several published studies.
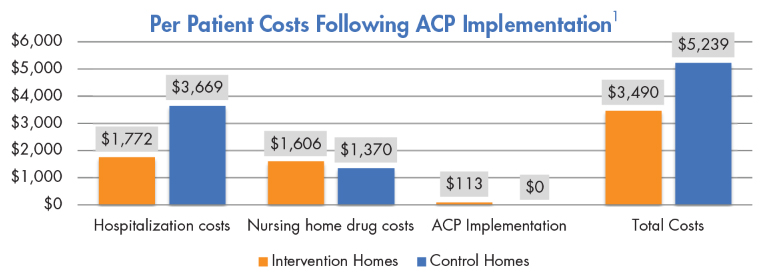
In a multisite randomized controlled trial of ACP in nursing homes, Molloy et al. found that
per patient health care costs were substantially lower in nursing homes that implemented the ACP intervention (average difference of $1749CAN; p=0.01).
1) Nursing homes that implemented the intervention also saw
fewer hospitalizations per patient (p=0.001) and a
lower average number of days spent in hospital (p=0.01).
In another study of the effects of a complex ACP program deployed in nursing homes, Levy et al. found that following implementation, residents were less likely to die in the hospital (48.2% pre-intervention versus 8.9% post-intervention, p<0.0001).
2) Every resident who died after ACP program implementation had an advanced directive (p=0.03), and
residents were more likely to be referred to palliative care (7.4% pre-intervention versus 31.1% post-intervention, p=0.02).

ACP impact on utilization was also seen in a study of the effects of end-of-life discussions between patients with advanced cancer and their physicians. Wright and colleagues found that
end-of-life discussions were associated with lower rates of ventilation (adjusted odds ratio [OR], 0.26 95% confidence interval [CI] 0.08, 0.83),
resuscitation (adjusted OR 0.16 1),
ICU admission (adjusted OR 0.35 2), and
earlier hospice enrollment (adjusted OR 1.65 3).
3) More aggressive medical care was associated with worse patient quality of life and higher risk of major depressive disorder in bereaved caregivers, whereas
longer hospice stays were associated with better patient quality of life.
Learn how the Coalition for Compassionate Care of California can help you
develop an advance care planning program through our consulting service.
Developed with support from the California Health Care Foundation.
 Kathleen Kerr is a healthcare consultant in private practice. She has expertise in palliative care, quality improvement and program evaluation, with particular interest in assessing financial outcomes. Her professional experience includes more than a decade of work as a senior analyst in the Department of Medicine at the University of California, San Francisco, where she participated in educational, technical assistance and research efforts focused on quality, safety, hospitalist financial and clinical outcomes, medical education and palliative care.
Kathleen Kerr is a healthcare consultant in private practice. She has expertise in palliative care, quality improvement and program evaluation, with particular interest in assessing financial outcomes. Her professional experience includes more than a decade of work as a senior analyst in the Department of Medicine at the University of California, San Francisco, where she participated in educational, technical assistance and research efforts focused on quality, safety, hospitalist financial and clinical outcomes, medical education and palliative care.