As a nursing home and palliative care physician, my work can be heart-wrenching. My patients and their families are often facing extremely difficult decisions as we walk the path of serious illness together. However, over the last 20 years I’ve found that taking my dogs with me to do patient care tends to lighten my load—and I know they have helped many of my patients too.
When a therapy dog enters the room the atmosphere automatically becomes more relaxed. As patients pet or snuggle with my dogs, they often share fond memories of their own beloved pets. This act of remembrance and storytelling transforms the care setting from what can be an intimidating, sterile environment into a place of positive, unconditional love.
A Doc and His Dogs
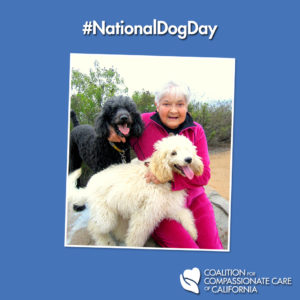
Tessa, a 10-year-old cockapoo, is my pet therapy dog. Both she and her younger counterpart in training, Josie—a spirited 2-year-old black miniature poodle—almost always bring a level of joy and comfort to patients in a way that I’m confident I could not achieve without them.
I often wonder what it is about dogs that helps patients open up in my presence. Perhaps it is because they are never judgmental over changes in appearance and they never shy away from a patient who is severely ill. And dogs are never startled by scars, wounds or smells that otherwise might make a patient feel self-conscious.
It is human nature to treat people differently when they are sick—even family members may feel uneasy when visiting ill loved ones—but dogs live in the moment, sharing joy regardless of the situation.
Dogs and the Elderly
Severely demented patients who have lost most of their mental capacities often seem to connect with dogs on a deeper level. These patients smile, laugh, and occasionally cry, as they run their fingers through my poodles’ curly hair. A patient may shy away from the offer of another person’s hug or a touch of the hand, but they gladly squeeze my dogs, pet their heads, and accept kisses and comforting physical contact with their canine visitors.
One of my fondest memories is back when Josie was still a puppy and in training. We were visiting one of my elderly patients and Josie started licking and nuzzling her in the ear. The sensation tickled her so much she let out genuine and exuberant laughter, which triggered alarm among the entire nursing staff who rushed in to see what was going on. Relieved, they commented that they had never heard this patient laugh like that at any time during her extended stay at their nursing facility. That patient is now 100 years old and still cherishes her visits with my dogs.
How it all Started…
I first started bringing Necca, my Dalmatian, to work with me in 1994. At the beginning I worried that her presence would seem undignified or not serious enough to be among my very ill patients. I soon came to realize that, except in rare instances, dogs added something extra to my patient interactions. While they may be a bit of a distraction, having dogs around during serious discussions (e.g., death and dying, hospice, control of severe symptoms, spiritual questions) injects warmth and love into the conversation. In thousands of such interactions over the last 20 years, I have never heard any patient or family member complain about it to me or to anyone else.
It's not all Unselfish
Some people might think it’s purely altruistic for me to take the dogs on rounds, but that is only part of the picture. Having them with me truly makes my day better, too. Yes, it can slow you down some; when you walk down the hall and someone shouts from a room, “Oh! A dog!”—I really can’t just walk on by without stopping to share the love.
As far as my credibility is concerned, the dogs create an almost unfair advantage on the assumption of my empathy and compassion. (I like to think those are, in fact, among my positive attributes as a clinician and human being, but I don’t think the dogs prove it… they are just a nice adjunct.) I like to say that if karma really exists, I hope I get credit for a small fraction of the good energy my dogs share with ailing people on a daily basis.
Perks of the Calling
One of the nice perks of being a nursing home and hospice doctor is that I don’t have a waiting room full of people and if I get slowed down or spend a few extra minutes at the bedside, it is not going to cause any serious problems. In fact, sometimes those “delays” turn into breakthrough moments for patients and their families. There is something positive to be said about “slow medicine”—low-tech, high-touch, etc.
When my dogs are occasionally unable to join me on rounds, it’s not just my imagination that people seem distinctly less enthusiastic to see me. And I totally get it—I would probably feel the same way.
I feel blessed to have a job where I am of service and doing something meaningful, and it is even more rewarding that I get to have my dogs accompany me and share in the joy they bring.
Karl Steinberg, MD, CMD, HMDC, is President of Stone Mountain Medical Associates, and is board certified in family medicine and hospice and palliative medicine, with a focus on long-term care geriatrics and palliative medicine. He is a certified medical director for skilled nursing facilities and hospices. Steinberg chairs the board of directors of the Coalition for Compassionate Care of California, serves on the board of AMDA (The Society for Post-Acute and Long-Term Care Medicine), and is past president of the California Association of Long-term Care Medicine (CALTCM), among many other professional organizations. He thinks he is best known for taking his two dogs to work with him nearly every day.