Demonstration Highlights
Features and Focus
The goal of the Demonstration was to test the Standards with a cohort of health plans (Plans) and CBPC providers (Providers) that deliver CBPC services that meet or exceed the Standards in two regions of California (Los Angeles and Sacramento). Participants included four Plans and the Providers that were contracted with the participating Plans to deliver CBPC services to Plan members. Throughout the course of the project, Plan and Provider participants attended virtual and in-person meetings to share experiences and promising practices on operational topics ranging from encouraging referrals to assessing patient-reported outcomes. Plan participants also collaborated to create a Universal Referral Form that referring providers (oncologists, hospitalists, etc.) could use to refer patients to any of the four Plans’ palliative care programs.
Evaluation
The Demonstration featured both quantitative and qualitative evaluations, which focused on evaluating outcomes and variation in care delivery, as well as the experiences of the Plans and Providers. A central question was if the financial outcomes were sufficient to make CBPC services sustainable for Plans and Providers.
Plans provided data describing patient demographics, palliative care enrollment, and use and cost of health care services. Providers shared tools and data used to assess patient experience of care. Plans and Providers shared oral and written information regarding policies, practices, and experiences delivering CBPC.
Three of the four Plans offered products in both Sacramento and Los Angeles. Two of the Plans only offered Medi-Cal (Medicaid) products. Two Plans started offering palliative care benefits upon implementation of the Medi-Cal requirement in January 2018, the other two Plans had been offering palliative care across multiple lines of business for several years. Plans were contracted with as many as 27 and as few as five palliative care providers in the two regions. All contracts met or exceeded the minimum requirements described in the Standards or the requirements for Medi-Cal palliative care (SB 1004) as described by the California Department of Health Care Services.
Eleven of the contracted palliative care providers participated in the Demonstration. These organizations had contracts with 1-3 of the participating Plans, and many also had contracts with payers that did not participate in the project. Providers cared for as few as 10 and up to >400 CBPC patients annually and had from 1 to >10 years of experience delivering CBPC.
Qualitative Evaluation
The qualitative evaluation focused on Plan and Provider perceptions of the acceptability of the Standards, as well as variation in how Plans and Providers enhanced or operationalized the Standards. Because the Standards defined minimum requirements and encouraged users to exceed those minimums, some variation was expected. However, many issues related to delivering CBPC are not addressed in the Standards, meaning that differences in approaches to implementing the Standards could create the kind of problematic variation that the Standards were designed to reduce.
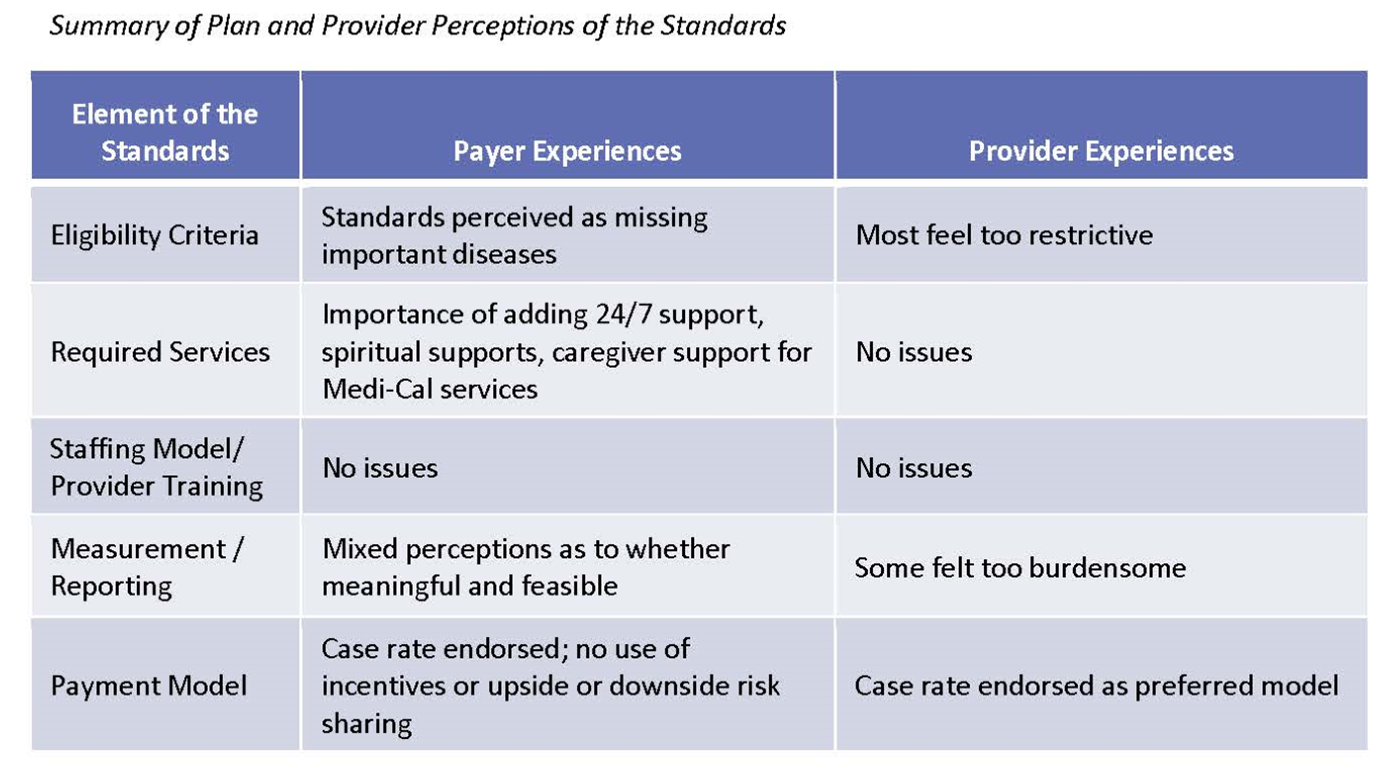
For each element of the Standards, Plans and Providers were invited to share their perceptions of the adequacy of the minimum requirements, from a clinical and operational perspective. Key questions included: Did the eligibility criteria identify the correct population, were the required services aligned with what patients and families needed, was the staffing model and provider qualifications appropriate, were the measurement and reporting requirements meaning and feasible, was the guidance on payment model appropriate? A summary of Plan and Provider perceptions is presented in the below table. More detail is available in the webinar recordings and presentation materials.
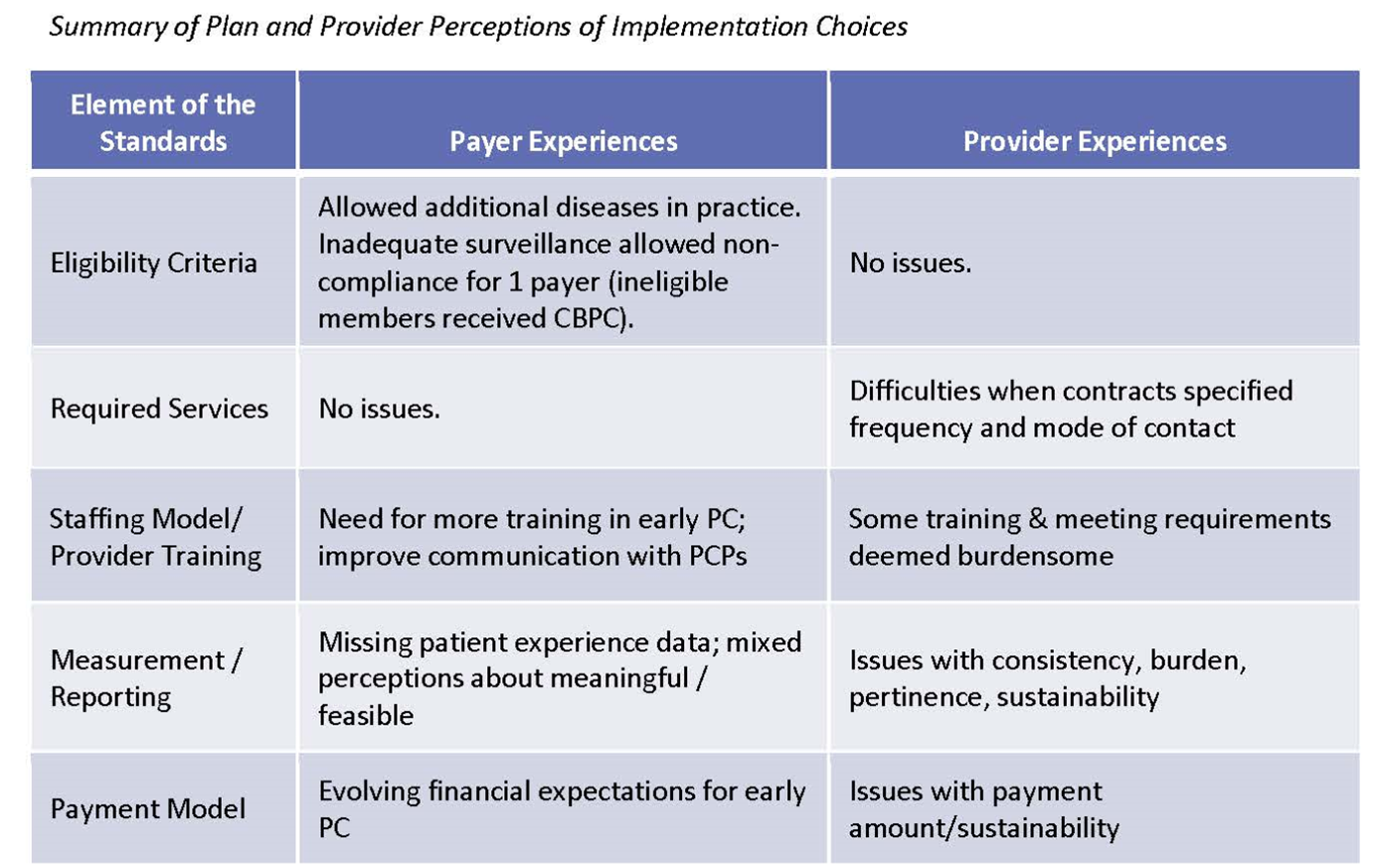
In addition, Plans and Providers shared perceptions about implementation issues related to elements of the Standards. The focus here was on choices Plans and Providers made about how to enhance or implement each element of the Standards, and the extent to which those choices impacted acceptability or sustainability from the Plan or Provider perspective. A summary of Plan and Provider perceptions is presented in the below table. More detail is available in the webinar recordings and presentation materials.
Quantitative Evaluation
Three Plans shared data describing enrollments in CBPC, member characteristics and care costs for 902 members who received CBPC between January 2019 and March 2020, across Medicare, Medi-Cal and commercial lines of business. Additional detail on quantitative analysis findings is available in the webinar recordings and presentation materials.
Enrollment
Plan data showed significant variation in enrollment duration across insurance types and across Plans.
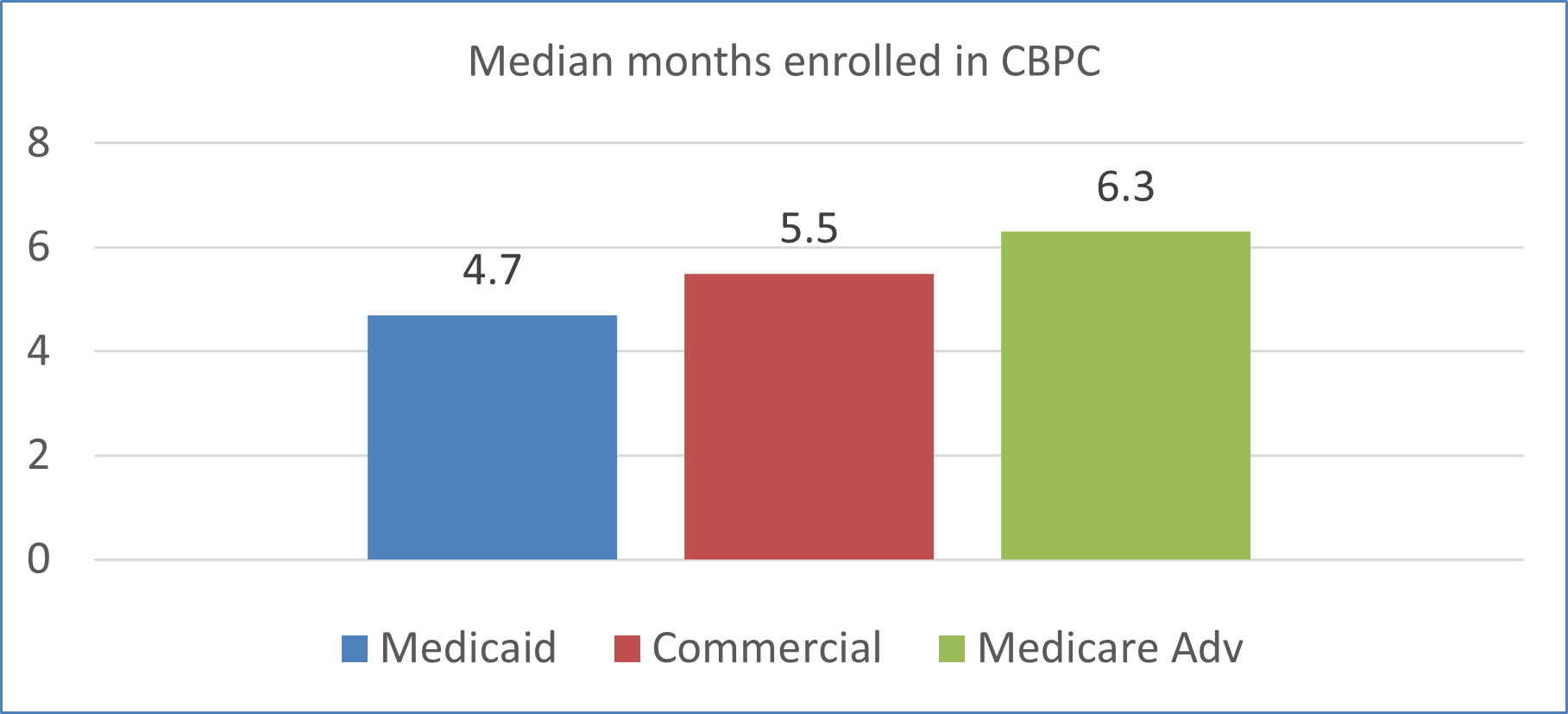
For the Medicaid, median enrolled months across the three Plans was 3.1, 5.7, 6.5 months, pointing to the impact implementation choices have on outcomes.
Fiscal impact
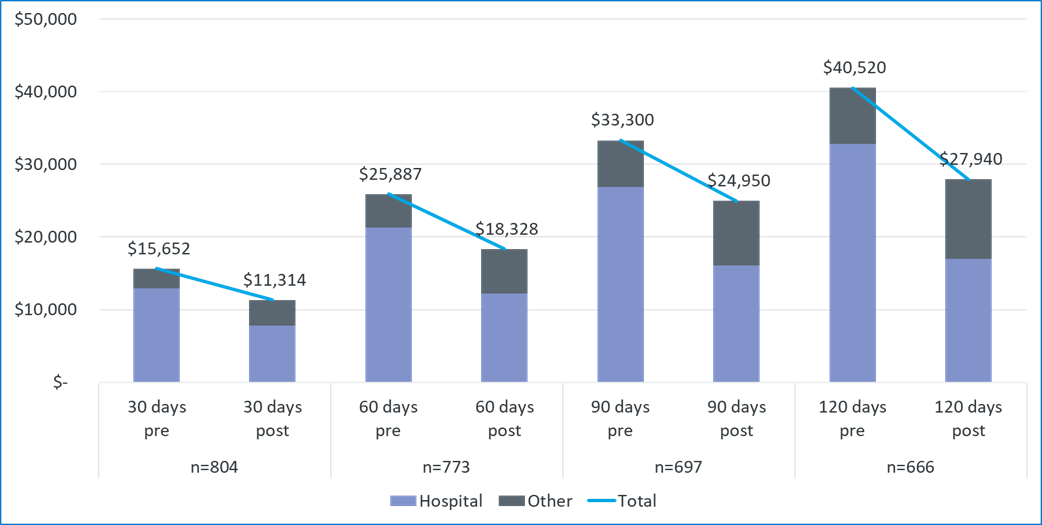
Data supplied by the Plans were used in a preliminary analysis of economic outcomes that compared costs before and after CBPC enrollment, using 95% confidence intervals to evaluate statistical significance. The analysis looked at four time periods: 30/60/90/120 days before and after enrollment. All expenditures were categorized as either “hospitalization-related” or “other.” Costs after PC enrollment are inclusive of CBPC payments, and of hospice claims for Medicaid and Commercial beneficiaries. Costs continue to accrue even if the person disenrolled from CBPC but remained with the Plan.
Looking at claims for all insurance types combined, this analysis showed that costs were reduced by 25% - 31% across the four time periods (all significant.)
Reflections
- The Standards were successful in promoting delivery of team-based care that aligned with expert consensus guidelines, setting a floor for contracting.
- Both Plans and Providers made use of flexibility to exceed the minimum requirements outlined in the Standards, such as expanding eligibility to include other patients with advanced disease.
- The evaluation found significant variation in how the Standards were enhanced and implemented. Some variation was manageable (expected), and some was problematic.
- Measurement and reporting was the area with the most problematic variation.
- Preliminary assessment of fiscal outcomes showed positive results.
- Both “what” (model/standards) and “how” (implementation choices) dictate outcomes.
Recommendations
Developing Standards
- Seek and incorporate input from a diverse group
- Define a floor (minimum) that reflects evidence-based best practices and allow for and encourage enhancements
- Balance specificity with ability to accommodate reasonable variation
Implementation Issues
- Use Standards as a starting point for contracting, to encourage use of best practices and reduce problematic variation
- Collect and share information about promising practices
- Create opportunities for peer-to-peer learning
Evaluation Issues
- Assess acceptability, feasibility, impact, and sustainability
- Make standards and evaluation findings easily accessible to all
- Use findings to inform on-going quality improvement